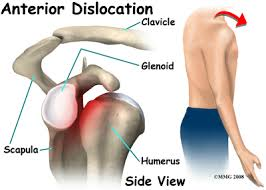
Anterior dislocation of the shoulder happens when the head of the humerus (upper arm bone) comes out of its usual position in the glenoid fossa, which is the socket part of the shoulder blade that holds the ball part of the upper arm bone. This type of dislocation is characterized by its forward direction; that is, the head of the humerus moves forward to the body. It’s the most common type of shoulder dislocation, often resulting from a traumatic injury such as a fall or a direct blow to the shoulder, or from forceful throwing or lifting. Symptoms include severe pain, swelling, immobility of the shoulder, and a visible deformity of the shoulder area. Immediate medical attention is required to return the humerus to its proper position, followed by rehabilitation to restore function and prevent future dislocations.
What is recurrent anterior dislocation of the shoulder?

Recurrent anterior dislocation of the shoulder involves the shoulder joint frequently dislocating toward the front of the body. This condition typically arises from an initial shoulder dislocation that compromises the joint’s stability. Over time, the ligaments and muscles around the shoulder may become stretched or torn, making it easier for the shoulder to dislocate again. Symptoms often include pain, instability, and a decreased range of movement. Management can involve physical therapy to strengthen the shoulder, or in some cases, surgery may be required to repair or tighten the damaged ligaments.
What causes recurrent anterior dislocation of the shoulder?
Recurrent anterior dislocation of the shoulder typically results from an initial dislocation that damages the stabilizing structures of the shoulder joint, making it more susceptible to subsequent dislocations. The key causes and risk factors include:
- Bankart Lesion: This is a tear of the labrum, which is a ring of cartilage that surrounds the socket of the shoulder joint. This tear can result from the initial dislocation and compromise the joint’s stability, making future dislocations more likely.
- Capsular Laxity: After a dislocation, the joint capsule (the connective tissue that surrounds the shoulder joint) can become stretched or torn, leading to increased laxity (looseness) in the joint. This laxity makes it easier for the shoulder to dislocate again.
- Hill-Sachs Lesion: A Hill-Sachs lesion is an indentation in the back of the humeral head (the ball of the shoulder joint) that occurs when the humeral head impacts the edge of the glenoid (the socket) during a dislocation. This defect can interfere with the normal mechanics of the shoulder and predispose it to redislocation.
- Rotator Cuff Injuries: The rotator cuff is a group of muscles and tendons that stabilize the shoulder. Damage to these tissues, either from the initial dislocation or from wear and tear over time, can decrease the shoulder’s stability.
- Repetitive Overhead Activities: Athletes or individuals who frequently engage in activities that involve overhead motions (e.g., volleyball, baseball, swimming) are at a higher risk of experiencing recurrent shoulder dislocations due to repeated stress on the shoulder joint.
- Genetics and Connective Tissue Disorders: Some people may have a genetic predisposition to more lax joints or connective tissue disorders, which can increase the risk of shoulder dislocations.
Treatment for recurrent anterior dislocation of the shoulder

Management of recurrent anterior shoulder dislocation may involve physical therapy to strengthen the muscles around the shoulder, techniques to improve proprioception (the sense of joint position), and, in some cases, surgical intervention to repair the damaged structures. Surgery aims to restore stability to the shoulder joint, correcting specific defects such as labral tears or capsular laxity.
The treatment for recurrent anterior dislocation of the shoulder typically involves both non-surgical and surgical options, depending on the severity of the condition and the patient’s lifestyle and activity level.
Non-surgical treatment
- Physical therapy: Exercises focusing on strengthening the rotator cuff muscles and improving shoulder stability and control.
- Activity modification: Avoid activities or movements that place the shoulder at risk of dislocation.
- Bracing or taping: Using a shoulder brace or tape to provide support and limit the range of motion during activities that could lead to dislocation.

Surgical treatment
Surgery is considered when non-surgical approaches fail to prevent recurrent dislocations or in cases of significant structural damage. Surgical options may include:
- Bankart repair: Surgery to repair torn ligaments in the shoulder and reattach them to the bone.
- Latarjet procedure: A bone graft is taken from the scapula or elsewhere and attached to the front of the shoulder socket to prevent dislocation.
- Capsular shift: Tightening the joint capsule to provide increased stability to the shoulder joint.
After surgery, a period of immobilization followed by physical therapy is crucial for recovery, regaining strength, and preventing future dislocations. The choice of treatment should be guided by the specific needs and goals of the patient, and it’s usually decided after a thorough assessment by an orthopaedic surgeon or a sports medicine specialist.
A word from the Hyderabad shoulder clinic
We would like to assure all our patients that Dr.Chandrashekhar B has decades of experience in handling recurrent anterior shoulder dislocation cases. You can rest assured that we will do everything, which includes diagnosis, treatment and future care, to avoid the recurrent anterior dislocation of the shoulder. For more information, please visit our website https://hyderabadshoulderclinic.com/ or contact us at +91 9959588389 or shoulderandsportsclinic@gmail.com.