Chronic shoulder instability refers to a condition where the shoulder joint is unable to maintain its normal position, leading to frequent dislocations or a feeling of looseness. This instability can be caused by various factors, including previous shoulder injuries, ligament laxity, or repetitive overhead activities. Individuals with chronic shoulder instability often experience pain, weakness, and a limited range of motion. Treatment typically involves physical therapy to strengthen the surrounding muscles, along with potential surgical options if conservative measures fail to provide relief.
Chronic shoulder instability surgery
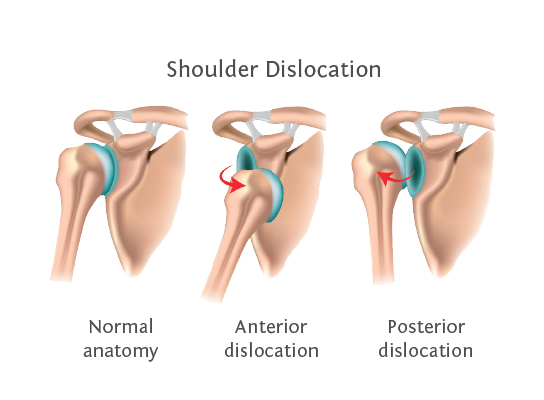
Surgical options for chronic shoulder instability typically aim to restore stability to the shoulder joint and reduce the risk of future dislocations. Common surgical procedures include:
Bankart Repair: This procedure involves reattaching the torn labrum and any damaged ligaments to the glenoid (the socket part of the shoulder) to improve stability.
Latarjet Procedure: This approach involves transferring a piece of bone from the shoulder blade to the front of the glenoid to create additional stability, often used in cases of significant bone loss.
Capsular Shift: This technique tightens the shoulder joint capsule by folding and suturing it, which can help reduce looseness.
Arthroscopic Stabilization: Less invasive than open surgery, this method uses small incisions and cameras to repair the structures around the shoulder.
Rotator Cuff Repair: If there are associated tears in the rotator cuff, repairing this can also help with overall shoulder stability.
Rehabilitation postsurgery is crucial for a successful recovery, focusing on restoring strength and range of motion. It’s important to discuss the best option with an orthopedic surgeon based on individual circumstances and the severity of instability.
Chronic shoulder instability surgery procedure
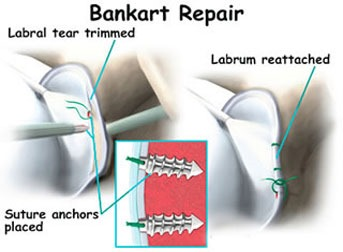
Chronic shoulder instability surgery typically involves a few key procedures aimed at restoring stability to the shoulder joint. One common surgical technique is called Bankart repair, which addresses a tear in the labrum (the cartilage that helps keep the shoulder joint stable) caused by repeated dislocations.
- Anesthesia: The surgery is usually performed under general anesthesia or regional anesthesia.
- Incision: The surgeon makes an incision either on the front of the shoulder (open surgery) or uses arthroscopic techniques that involve smaller incisions.
- Accessing the Joint: If using arthroscopy, a camera (arthroscope) is inserted through one incision, which allows the surgeon to view the joint on a monitor. Other instruments are inserted through additional small incisions.
- Repairing the Labrum: The surgeon will locate the Bankart lesion (the tear in the labrum) and reattach the labrum to the glenoid (the socket part of the shoulder) using sutures or anchors.
- Reinforcing Stability: If necessary, the surgeon may also tighten the ligaments around the shoulder joint or perform procedures on associated structures, such as the capsule surrounding the joint.
- Closure: Once the repair is complete, the incisions are closed, either with sutures or staples, and a bandage is applied.
- Rehabilitation: Postsurgery, patients usually undergo a rehabilitation program that includes physical therapy to restore strength and mobility to the shoulder.
It’s crucial for patients to follow their surgeon’s postoperative care instructions and attend all followup appointments to ensure proper healing. The goal of the surgery is to reduce or eliminate shoulder dislocations and improve overall shoulder function.
Advice from Hyderabad Shoulder clinic about Chronic shoulder instability surgery rehabilitation

Chronic shoulder instability surgery rehabilitation typically involves several phases to ensure effective recovery and restoration of function. Here’s a general outline of what the rehabilitation process may look like:
Phase 1: Immediate PostOperative (02 weeks)
- Goals: Pain control, protect the surgical repair, and begin gentle passive motion.
- Activities:
- Use a sling for protection.
- Engage in passive range of motion (ROM) exercises as advised by the surgeon.
- Begin ice therapy to manage swelling and pain.
- Avoid any active movements or loading of the shoulder.
Phase 2: Early Rehabilitation (26 weeks)
- Goals: Gradual restoration of shoulder motion and strength.
- Activities:
- Continue using the sling as necessary.
- Progress to active assisted ROM exercises.
- Begin isometric contractions (such as activating the shoulder muscles without moving the joint).
- Maintain workout for other areas to prevent overall deconditioning.
Phase 3: Intermediate Rehabilitation (612 weeks)
- Goals: Increase strength, ROM, and begin functional activities.
- Activities:
- Gradually wean off the sling as approved by the physician.
- Introduce active ROM exercises.
- Start light resistance training and strengthen the rotator cuff and scapular stabilizers.
- Engage in neuromuscular control exercises (like using a balance board).
Phase 4: Advanced Rehabilitation (36 months)
- Goals: Restore full strength and return to sports or activities.
- Activities:
- Focus on more sportspecific exercises and functional tasks.
- Incorporate Plyometrics and dynamic stability exercises.
- Start a more progressive strengthening program with resistance bands or weights.
- Perform activities that mimic the patient’s sport or daily activities.
Phase 5: Return to Sport/Activity (612 months)
- Goals: Full return to preinjury level of activity or sport.
- Activities:
- Gradually return to full activity as recommended.
- Include advanced conditioning, agility drills, and sportspecific practice.
- Continue with a home exercise program to maintain shoulder strength and stability.
Important Tips from Dr.Chandra Sekhar B, of Hyderabad Shoulder clinic
- Always follow the surgeon’s guidelines regarding the timeline and type of exercises.
- Work closely with a physical therapist throughout the rehabilitation process.
- Listen to your body and avoid pushing through pain during recovery.
- Regular followup appointments are crucial to monitor progress and make necessary adjustments to the rehabilitation program.
This is a general guide, and individual rehabilitation protocols may vary based on specific surgical procedures and individual patient needs. Always consult us at Hyderabad Shoulder clinics for personalized recommendations.For more information, please visit our website https://hyderabadshoulderclinic.com/ or contact us at +91 9959588389 or shoulderandsportsclinic@gmail.com.